Provider Credentialing First Truth for New Medical Practice
Starting a new medical practice can be exciting and full of enthusiasm. However, it’s essential to remember that a significant amount of groundwork needs to be completed. Among the myriad of tasks on the to-do list, healthcare provider credentialing stands out as one of the first and most fundamental. Physicians need it to join insurance networks and for the new medical practice to get paid for its services. Let’s dive deep into why provider credentialing is crucial, especially for a fledgling practice.
What is Provider Credentialing?
Specifically, making sure that healthcare providers are legit is a big deal. Provider credentialing checks their background and qualifications to ensure they’re the real deal. Hence, this process ensures that physicians meet the necessary standards to treat patients. Accordingly, it’s a safeguard that protects patients and maintains the integrity of the healthcare system by ensuring that only qualified and competent providers are part of it.
Why Provider Credentialing Matters for a New Medical Practice
After all, starting a new practice comes with its set of challenges and opportunities. Therefore, one of the primary steps involves ensuring that every provider is properly credentialed. Here are several reasons why this is vital:
Ensuring Quality of Care
Chiefly, the credentialing process verifies a provider’s education, training, experience, and competency. Likewise, it evaluates their ability to deliver high-quality care to patients. For a new medical practice, establishing a reputation for excellent care is pivotal. Furthermore, effective provider credentialing helps to ensure that the physicians in the practice meet stringent standards and are capable of providing the best possible care.
Legal and Regulatory Compliance
For instance, medical practices are subject to numerous legal and regulatory requirements. Undoubtedly, provider credentialing helps ensure compliance with healthcare laws and regulations. It reduces the risk of legal issues arising from unqualified or inadequately checked providers. Non-compliance not only tarnishes a practice’s reputation but can also lead to costly fines and sanctions.
Insurance Reimbursements
Insurance companies require providers to be credentialed before they can bill and receive payments for their services. Of course, without this accreditation, a new medical practice could face severe financial challenges, as insurance reimbursements form a significant portion of its revenue. Therefore, effective credentialing facilitates smooth reimbursement processes and ensures that the practice can sustain itself financially.
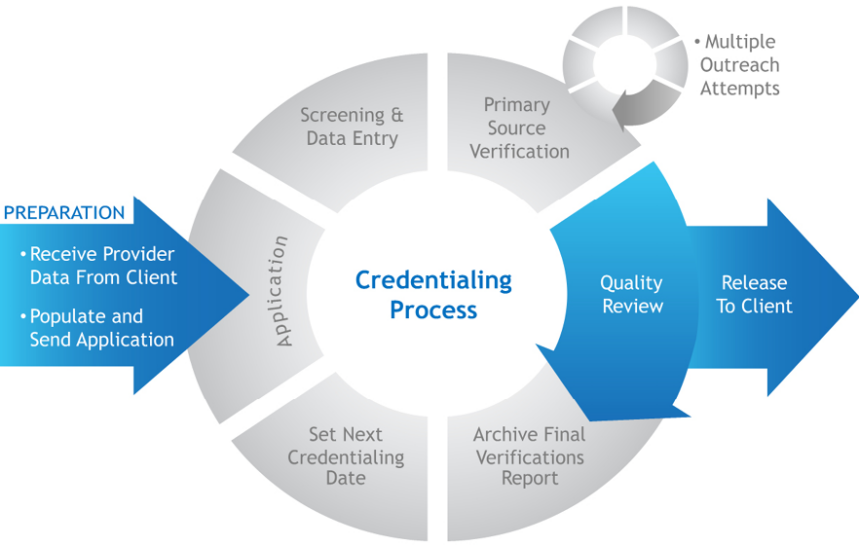
The Provider Credentialing Process: Step-by-Step
While the credentialing process might seem daunting, breaking it down into manageable steps can make it more approachable:
Gathering Information
The first step in provider credentialing involves collecting detailed information about the physicians. Of course, this includes their educational background, training, work experience, certifications, licenses, and references. Accurate and thorough documentation is crucial during this phase.
Verification
The next step involves verifying all the information gathered. Of course, this means cross-checking degrees, licenses, certifications, and any claims of work experience. Various databases and agencies, such as the National Practitioner Data Bank (NPDB), are used during this stage to ensure accuracy and authenticity.
Review and Approval
After verification, the information is reviewed by credentialing committees within insurance companies or healthcare organizations. Additionally, they assess whether the physician meets their standards and requirements. Furthermore, approval at this stage allows the provider to be added to insurance networks, enabling the practice to bill for their services.
Maintaining Credentials
Credentialing is an ongoing process. Furthermore, providers must periodically update and maintain their credentials, ensuring that their certifications and licenses are current. Regular re-credentialing ensures that the standard of care remains high and compliant with evolving regulations.
Simplifying Provider Credentialing with Technology
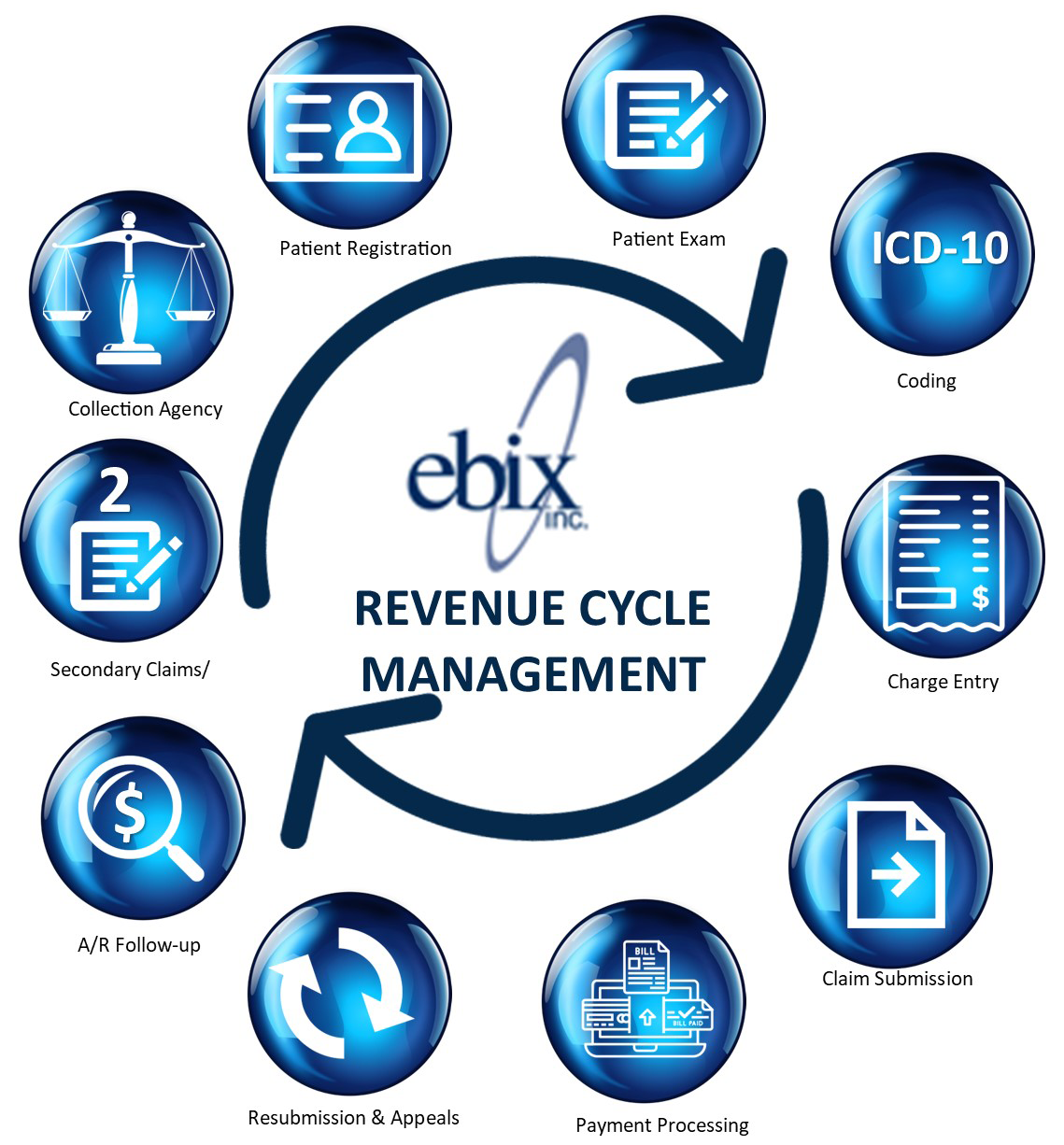
In today’s digital age, technology plays a vital role in simplifying complex tasks. Credentialing is no exception. Platforms like Ebix offer comprehensive solutions to streamline the provider credentialing process for new medical practices.
Why Choose ebix, Inc. for Credentialing?
Actually, ebix, Inc. is a renowned provider of cloud-based solutions for the healthcare industry. Using their credentialing services can offer numerous benefits:
1. Efficiency: The ebix, Inc. team significantly speeds up the credentialing process by automating time-consuming tasks such as data collection and verification.
2. Accuracy: With sophisticated algorithms and extensive databases, the ebix, Inc. team ensures that all information is accurate and verified.
3. Compliance: The ebix, Inc. team incorporates the latest regulations and standards into its processes, ensuring that your practice remains compliant at all times.
4. Cost-Effective: By streamlining the credentialing process, the ebix, Inc. team reduces the administrative burden, allowing your practice to allocate resources more effectively.
Tips for Navigating the Credentialing Process
Even with the best technology at your fingertips, understanding the intricacies of credentialing can be beneficial. Here are some handy tips:
Plan Ahead
Credentialing can take anywhere from a few weeks to several months. Starting the process early can prevent delays in launching your practice. Being proactive ensures that all necessary documentation is ready and complete when needed.
Stay Organized
Maintaining a well-organized system for credentialing documentation is crucial. Digital tools and platforms like ebix, Inc. can assist in creating and managing a centralized database for all credentials, making it easier to track and update information as required.
Continuous Education
Healthcare is an ever-evolving field. Keeping abreast of new regulations, standards, and best practices in credentialing is essential. Regular training and updates can help ensure that your practice remains compliant and provides the best possible care.
The Impact on Patients
Ultimately, the benefits of thorough provider credentialing extend beyond the practice; they significantly impact patients. Ensuring that only qualified and competent physicians provide care fosters trust and confidence in the practice. Patients can feel secure knowing that their healthcare providers have met stringent standards, leading to better health outcomes and patient satisfaction.
Credentialing as a Building Block
Starting a new medical practice is like constructing a building. Each aspect, from securing a location to hiring staff, is a brick in the foundation. Provider credentialing is one of the fundamental steps in this construction process. It’s a vital block that must be placed with precision and care to support the entire structure. By prioritizing and effectively managing provider credentialing, a new practice sets the stage for success, growth, and the delivery of exceptional patient care.