Skilled Nursing Facility Billing – When You Need to Optimize
Nursing, until 1998, nurse center billing was easy since skilled nurse facilities (SNFs) could bill separately for their service. Since 1998, after the BalancedBudget Act came into effect, several things about how SNFs claim reimbursement have changed. The points below will outline the changes:
Challenges of Skilled Nursing Facility Billing
 Producing SNF claims as part of consolidated billing requires the knowledge of codes and familiarity with what is covered by Medicare A and what is not. If Medicare A does not protect something, then it may be covered by Medicare B. The SNF has to identify that and bill it separately.
Producing SNF claims as part of consolidated billing requires the knowledge of codes and familiarity with what is covered by Medicare A and what is not. If Medicare A does not protect something, then it may be covered by Medicare B. The SNF has to identify that and bill it separately.
On the other hand, payment on a per diem basis means a fixed amount CMS pays to SNFs under Medicare A, with which SNFs pay contracted nursing service providers for their services.
- Now SNFs have to produce their claim as part of consolidated billing under the Prospective Payment System (PPS)
- Medicare A pays SNFs on a per diem basis
Nursing Facilities Billing Challenges are:
- The inaccuracy of codes applied to lead to the rejection of claims
- Insufficiency of knowledge of items covered by Medicare A and B
- Fixed or per diem payments for services not accommodating cost borne by the nursing facility adequately – given that there is a degree of cost elasticity in the range of services offered by facilities, which the fixed rates often fail to encompass
The above two scenarios expose nursing facilities to two kinds of revenue leakage: via rejected claims and through the underpayment of services.
Additionally, it’s often difficult to establish that the patient requires the services provided by a nursing facility and excessive time spent on non-medical activities.
Outsourcing Skilled Nurse Facility Billing to ebix, Inc
The ebix, Inc. team has helped nursing centers in rural and urban areas throughout the Midwest to improve their revenues by reducing reimbursement rejection rates and increasing their focus on nursing services. The ebix, Inc. team has extensive knowledge of billing and coding intricacies. From identifying patient: eligibility for reimbursement to accurately separating items covered by Medicare A and Medicare B. They also perform post-claim-submission follow-ups to ensure timely repayment of payments by CMS.
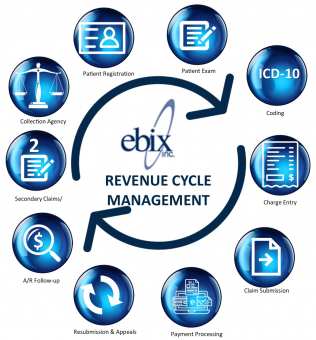
Our outsourcing model includes the entire billing and coding activities, from identifying the patient’s insurance eligibility to submission of claims and post-submission follow-ups.
Our Revenue Cycle Management model involves a thorough study of your revenue management cycle to spot areas of revenue leakage and plugs them by helping reduce outdated or cumbersome processes and assist in replacing inept software applications with new ones customized to your need and environment along with help in training people where required.
Skilling Nursing Facility Billing Services for Your Practice
- Initial Credentialing is Free. Our expert staff reaches out to the carriers of your choice to obtain network status. Namely, accessible at a startup and a very reasonable fee per provider afterward.
- Fee Schedule Analysis. We enter the allowed amounts from the network contracts obtained to track and uncover any improper reimbursements. We will help research appropriate change levels.
- Workflow Consulting. Our management staff has over 100 years of combined experience. Therefore, we can advise you on the best practices to build a team and processes that ensure results.
- Carrier Contract Advice. Consequently, there are pitfalls to avoid in contracts and situations that may cause you to choose non-network status with challenging carriers. We have additional expert resources to bring help when necessary.
- Coding Expertise. The ebix team offers certified coding staff to “abstract” codes from provider documentation or review your code for accuracy and completeness. We offer Chart auditing services and provider/staff education. Additional revenue opportunities, compliance, and audit survival are the results of our efforts.
- Fees based on Results. We don’t get paid until we’ve obtained reimbursement for you.
- No Surprises. No additional charges for postage, claims, statements, or custom report/data analytics needs.
- Fast Claim Submission. Your billing will be submitted promptly after receipt. Don’t suffer from delays or write-offs from inappropriate submissions.
- Up to 10% Better Reimbursements.
Medical Coding Compliance
By and large, medical billing begins with accurate and complete documentation in the medical record. Hence, coding is how your intellectual services and labor translate into a code used to bill insurance and document the value of your service. The ebix Skilled Nursing Facility Billing team has a strong reputation as an expert in medical coding service.
Perhaps most noteworthy are the ICD-10 codes. The ICD-10 is currently the cornerstone of classifying diseases, injuries, health encounters, and inpatient procedures in morbidity settings. Because of this, the ebix, Inc. team has honed medical coding skills and business processes to meet the needs of independent physicians.
Therefore, transforming a provider’s narrative or description of the disease, injury, and procedures into universal medical code numbers for the insurance claim is the fundamental purpose of medical coding. For this reason, our team of professional certified medical coders ensures higher reimbursement by properly aligning services with a medical diagnosis. Consequently, this doesn’t just assure proper payment. It will also minimize denials resulting from the incorrect association of diagnosis and procedure codes.
Data Analytics
Our financial reporting gives you the insight you need to address the root causes of charge issues, resolve process inefficiencies, improve coding compliance, and ensure the integrity of all claims. Office Managers and Administrators can quickly review performance and trends, drill down into the data to analyze root causes by reason, evaluate payer performance, and the financial impact of claim denials.
Examples of some of the financial reports we provide (above and beyond the regular month-end reporting that gives details about charges, collections, and your AR) include:
- Charge & Revenue Analysis – evaluate financial ratios versus MGMA benchmarks
- Coding analysis – identify potential under, over, and incorrect coding scenarios
- Procedure Analysis – analyze top CPT codes for cost-benefit analysis
- Payer Reimbursement Analysis – assess which payers consistently slow up payments through unnecessary denials and “lost” claims.
- Provider & Staff Productivity Analysis – evaluate provider and staff productivity based on the specific place of service, revenue, and RVUs
- AR Aging Analysis – velocity of payments per payor and CPT, respectively
Minimize Medical Claim Denials
Based on our experience working with physicians and healthcare organizations, we understand that the revenue cycle success starts at patient registration and continues throughout the claims cycle. Accuracy of patient demographics and financial information upfront results in reduced denials, fewer rejected claims and more occasional returned statements. Claim cleanliness is the critical component that stops the denial from origination, and the following parameters impact it:
- Patient registration data quality
- Prior-authorizations
- Non-covered services and medical necessity management
- Eligibility and benefits coverage
- Clinical documentation quality
- Coding
- Claim editing
- Payor rules & mandates