Denial Prevention – What You Need to Know Now
Denial Prevention Strategies: Based on our experience working with physicians and healthcare organizations, we understand that the revenue cycle success starts with patient registration and continues throughout the claims cycle. Accuracy of patient demographics and financial information upfront results in reduced denials, fewer rejected claims, and more occasional returned statements. Claim cleanliness is the critical component that stops the denial from origination, and the following parameters impact it:
- Patient registration data quality
- Prior-authorizations
- Non-covered services and medical necessity management
- Eligibility and benefits coverage
- Clinical documentation quality
- Coding
- Claim editing
- Payer rules & mandates
The ebix, Inc. team supports your healthcare organization with denial prevention capabilities and best practices. We’ll be able to help you find root causes for errors in the front end of your revenue cycle, improving the downstream process. In addition, we help check the medical necessity requirements and the creation of necessary ABNs, resulting in reduced denials and faster payments.
Experienced Billing Services get you more with Denial Prevention.
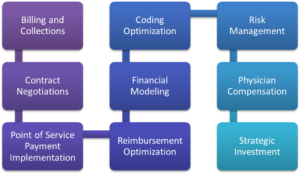
It is essential to realize that the key to successful Revenue Cycle Management is understanding all your practice’s revenue sources. Hence, our team will help improve profitability by monitoring, measuring, and managing all aspects of your revenue cycle.
Indeed, the ebix team has excellent tools and experience. Hence, our Revenue Cycle Management solutions are in place to capture revenue from claims remittances, patients, and evidence-based data. Collecting from all these sources will help secure your practice’s healthcare payments and make it more profitable.
Medical Coding Compliance

By and large, medical billing begins with accurate and complete documentation in the medical record. Hence, coding is how your intellectual services and labor translate into a code used to bill insurance and document the value of your service. The ebix team has a strong reputation as an expert in medical coding services.
Perhaps most noteworthy are the ICD-10 codes. The ICD-10 codes are currently the cornerstone of classifying diseases, injuries, health encounters, and inpatient procedures in morbidity settings. Because of this, the ebix, Inc. team has honed medical coding skills and business processes to meet the needs of independent physicians.
Therefore, transforming a provider’s narrative or description of the disease, injury, and procedures into universal medical code numbers for the insurance claim is the fundamental purpose of medical coding. For this reason, our team of professionally certified medical coders ensures higher reimbursement by properly aligning services with a medical diagnosis. Consequently, this doesn’t just assure proper payment; It will also minimize denials resulting from the incorrect association of diagnosis and procedure codes.