Physician Billing – When You Need to Maximize Now
We aim to be your go-to partner in enhancing your revenue and profitability as a physician by strategically optimizing your billing processes.
Starting to bill for any specialty can be challenging due to the learning curve involved. Providers and billing staff often find it tough to navigate through ever-changing payor rules and mandates, specialty coding, and billing requirements. Sometimes, billers rely on providers to share appropriate CPT and ICD codes, but providers may not always be up to date with the latest coding guidelines. This lack of knowledge and coding experience can negatively impact your receivables. At ebix, Inc., we understand that each specialty comes with its own set of challenges. Therefore, we work to develop custom workflows and a unique set of coding rules based on the services provided by your healthcare organization.
We are silent partners with specialty physicians in the following medical practices.
Anesthesiologists Cardiology Cardiothoracic & Endovascular Surgery Chiropractic Services Emergency Medicine Family Medicine Geriatric Medicine Gastroenterology Hospitalist Infectious Disease Internal Medicine OB/GYN Orthopedic Surgery Pain Management Pediatrics Physical Therapy Plastic Surgery Podiatry Pulmonology Radiology Urgent Care Urology And many more…
 Today, managing the business side of medical practice has become more expensive and time-consuming due to increasingly complex regulations and decreasing reimbursements. If you are running a private practice and looking for a new medical billing service, ebix, Inc. is the answer. Our detail-oriented team thoroughly understands all the codes and modifiers. We can help you improve your revenue.
Today, managing the business side of medical practice has become more expensive and time-consuming due to increasingly complex regulations and decreasing reimbursements. If you are running a private practice and looking for a new medical billing service, ebix, Inc. is the answer. Our detail-oriented team thoroughly understands all the codes and modifiers. We can help you improve your revenue.
Accordingly, ebix, Inc. is a trusted advisor to our clients in protecting their financial future. As a leading medical billing company, we know how to position our client’s practices for sustainable and immediate success within their industry. You may be pleased to know that we also have our proprietary billing software that effortlessly adapts to industry changes. Whether you want to enhance operational performance or increase revenue, we have your back.
Physicians Require Experienced Medical Billing Services.
- Initial Credentialing is Free. Our expert staff reaches out to the carriers of your choice to obtain network status. Namely, accessible at a startup and a very reasonable fee per provider afterward.
- Fee Schedule Analysis. We enter the allowed amounts from the network contracts obtained to track and uncover any improper reimbursements. We will help research appropriate change levels.
- Workflow Consulting. Our management staff has over 100 years of combined experience. Therefore, we can advise you on the best practices to build a team and processes that ensure results.
- Carrier Contract Advice. Consequently, there are pitfalls to avoid in contracts and situations that may cause you to choose non-network status with challenging carriers. We have additional expert resources to bring help when necessary.
- Coding Expertise. The ebix team offers certified coding staff to “abstract” codes from provider documentation or review your code for accuracy and completeness. We offer Chart auditing services and provider/staff education. Our efforts result from additional revenue opportunities, compliance, and audit survival.
- Fees based on Results. We don’t get paid until we’ve obtained reimbursement for you.
- No Surprises. No additional charges for postage, claims, statements, or custom report/data analytics needs.
- Fast Claim Submission. Your billing will be submitted promptly after receipt. Don’t suffer from delays or write-offs from inappropriate submissions.
- Up to 10% Better Reimbursements.
A Physician Needs Medical Coding Compliance
The ebix Billing Services team has a strong reputation as an expert in medical coding services. By and large, medical billing begins with accurate and complete documentation in the medical record. Hence, coding is how your intellectual services and labor are translated into a code used to bill insurance and document the value of your service.
Perhaps, most noteworthy are the ICD-10 codes. The ICD-10 is currently the cornerstone of classifying diseases, injuries, health encounters, and inpatient procedures in morbidity settings. Because of this, the ebix, Inc. team has honed medical coding skills and business processes to meet the needs of independent physicians.
Therefore, transforming a provider’s narrative or description of the disease, injury, and procedures into universal medical code numbers for the insurance claim is the fundamental purpose of medical coding. For this reason, our team of professional certified medical coders ensures higher reimbursement by properly aligning services with a medical diagnosis. Consequently, this doesn’t just assure you that you will be reimbursed. It will also minimize denials resulting from the incorrect association of diagnosis and procedure codes.
A Physician Needs Informative Data Analytics
Our financial reporting gives you the insight you need to address the root causes of charge issues, resolve process inefficiencies, improve coding compliance, and ensure the integrity of all claims. Office Managers and Administrators can quickly review performance and trends, drill down into the data to analyze root causes by reason, evaluate payer performance, and the financial impact of claim denials.
Our financial reports are more than just the standard month-end reports that detail charges, collections, and AR. We offer a range of detailed reports that can provide you with valuable insights into your financial performance. If you’re looking to make informed decisions and take your business to new heights, our reports can help you achieve that. For example, the following reports will help you see your business progress.
- Charge & Revenue Analysis – evaluate financial ratios versus MGMA benchmarks
- Coding Analysis – identify potential under, over, and incorrect coding scenarios
- Procedure Analysis – analyze top CPT codes for cost-benefit Analysis
- Payer Reimbursement Analysis – assess which payers consistently slow up payments through unnecessary denials and “lost” claims.
- Provider & Staff Productivity Analysis – evaluate provider and staff productivity based on the specific place of service, revenue, and RVUs
- AR Aging Analysis – velocity of payments per payer and CPT, respectively
A Physician Benefits from Minimized Medical Claim Denials
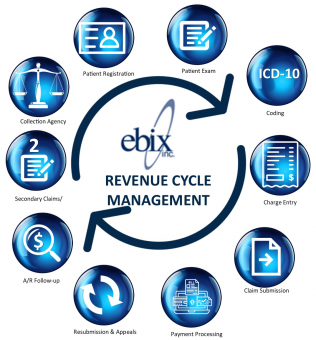
Specifically, based on our experience working with physicians and healthcare organizations, we understand that the revenue cycle success starts at patient registration and continues throughout the claims cycle. Accuracy of patient demographics and financial information upfront results in reduced denials, fewer rejected claims and more occasional returned statements. Claim cleanliness is the critical component that stops the denial from origination, and the following parameters impact it:
- Patient registration data quality
- Prior-authorizations
- Non-covered services and medical necessity management
- Eligibility and benefits coverage
- Clinical documentation quality
- Coding
- Claim editing
- Payor rules & mandates
We strive to maximize physician revenue through proactive Revenue Cycle Management, Predictive Analytics, and MIPS Compliance.
Additional Reading:
Billing Services: The Truth About Why Doctors Outsource