How to Reduce Claim Denials -Explode Revenue Now
Claim appeals are when you challenge a payer’s decision to deny reimbursement for a healthcare service or treatment. Here’s a proven How To approach to minimize issues.
If an insurance claim is denied, it is possible to file an appeal to contest the decision. In certain circumstances, the insurance company can be persuaded to reverse its initial decision. To appeal, you have to provide more information, documents, or evidence to support your claim and ask for the original decision to be reconsidered. There are different levels of appeals available to each payer, all with specific requirements and deadlines.
Looking for a more efficient process to handle denials and appeals? Read below for more tips and details about the way ebix, Inc.’s medical billing services team tackles denials and appeals.
First, ebix, Inc. assigns a medical billing specialist to your practice to work on any claim denials from a payer. The assigned specialist follows through with the steps below.
How to Understand the Reasons for Denial
Understanding the specific reason behind the insurance company’s denial is crucial when beginning the appeals process. This could relate to factors such as medical necessity, coding, or LCD guidelines. Clarifying this rationale will help to inform the subsequent steps in the appeals process. When you get the Explanation of Benefits with denial codes, the decision about the claim is fully documented. If the explanation remains unclear, the payer is contacted directly. Medical providers have the right to get claim denial information, and payers must explain it clearly.
How to Address Simple Problems
Claim denials can stem from numerous factors, with data entry errors being among the most frequent. Errors can include misspelled names, incorrect insurance policy numbers, and mismatched dates of services. A proven strategy is crucial to thoroughly examine the documentation furnished by the insurance company and scrutinize it for any errors. If discrepancies are found, ebix, Inc.’s medical billing specialist notifies the insurance company representative for rectification purposes. The claim is corrected and resubmitted for payer adjudication.
How to Gather Evidence
Unnecessary denials of claims can also arise due to the provision of services that are not deemed medically necessary. To avoid problems, it’s important to have enough proof and documentation for the treatment or services being offered, so you don’t have to show their medical necessity later. Referrals and other pertinent information regarding the patient’s medical history can aid in the approval of the claim. A proven strategy is to consult the health plan’s policy or guidelines for the services being billed. They are usually available online through the payer portals. This can help ensure that the services are being billed correctly and following the plan’s requirements. By referring to the policy or guidelines, it can help avoid any potential issues or discrepancies with the billing process.
Efficiency is Key
The ebix, Inc. team offers medical billing services that include storing all medical billing paperwork securely in a HIPAA-compliant portal. This proven strategy ensures efficient organization and transparency throughout the billing process. The billing paperwork is systematically sorted and stored in clearly labeled folders with appropriate file naming conventions for effortless access and management, which includes payer information, patient name, and date of service.
Completing the Necessary Paperwork
Another proven strategy is the appeal letter should be carefully crafted using a specific template tailored to the CPT code and payer. After finishing, send the letter quickly by fax or upload it to the payer portal. Make sure to include the claim number and relevant patient information. Payers frequently prioritize the processing of appeals when they are submitted using their designated forms or online portals. Additionally, the appeal process may be outlined in the EOB from the insurance company.
Denial Prevention: Key Information from the ebix, Inc, Team
To prevent denials, it is important to focus on patient registration and the claims cycle. This is based on our experience working with doctors and healthcare organizations. Ensuring the precision of patient demographics and financial information from the start leads to a decrease in claim denials, a lower number of rejected claims, and fewer instances of statements being returned. Claim cleanliness is the critical component that stops the denial from origination, and the following parameters impact it:
- Claim data quality
- Prior-authorizations
- Insurance coverage eligibility
- Clinical documentation quality
- Coding
- Claim editing
- Payer requirements
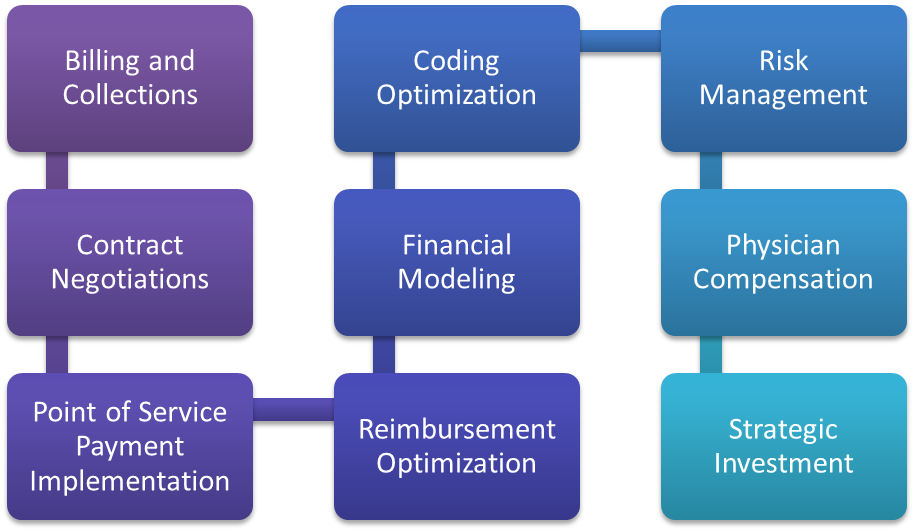
Our team at ebix, Inc. is dedicated to providing your healthcare organization with comprehensive denial prevention capabilities and best practices. We can help you identify why there are errors in the front end of your revenue cycle, which will improve the rest of the process. We also assist with checking medical necessity and creating necessary ABNs, leading to fewer denials and quicker payments.