Provider Credentialing: What You Need to Know Now
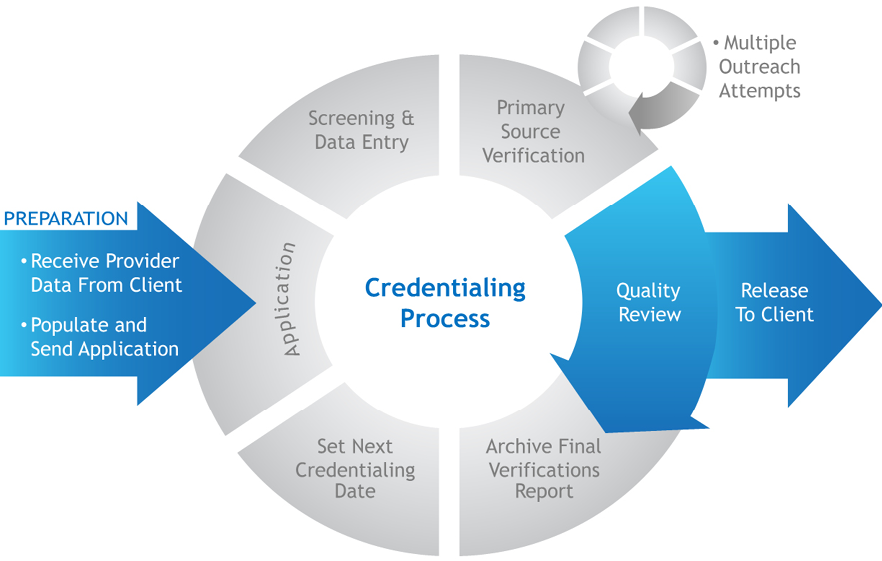
Provider credentialing is the process insurers use to verify a healthcare provider’s licenses, education and training, and background so the provider can be paid for covered services while supporting patient safety.
Key Takeaways: Provider Credentialing Services
- Credentialing is the foundation for working with both government and private payers; it establishes Payer Enrollment, reimbursement terms, and billing rules.
- During credentialing (which supports medical staff’s clinical privileges), providers typically enter into payer contracts that define reimbursement rates and billing guidelines.
- ebix, Inc. manages credentialing tasks, including primary-source verification of licenses and IDs (DEA, NPI), collection of required documents, submission of payer applications, and follow-up through approval.
- ebix, Inc. also supports ongoing maintenance, including tracking approvals and handling re-credentialing as needed.
Our expert staff contacts the carriers of your choice to obtain network status. It is free at startup and a very reasonable fee per provider afterward.
Provider Credentialing Overview
- Verification Process: verify credentials
- Collect documents
- Submit applications
- Payer follow up
- Confirm Verification Process and maintain
Insurance carriers use provider credentialing to assess the medical qualifications of healthcare providers and ensure they can receive payment for their services. It’s a thorough process to ensure the healthcare provider you see is qualified to provide the care you need. Always ensure that your healthcare provider has completed this process before seeking medical services from them. It’s the first step—and the foundation—for all your interactions with governmental and private payers. It’s the process insurance companies employ to verify your physician’s licenses, education, background, and other information.
Furthermore, as you go through the provider credentialing process, you’ll create a contract that establishes reimbursement rates and billing guidelines. Notably, this is a significant opportunity to ensure that your compensation is fair and accurately reflects the value of your services. Consider collaborating with your colleagues to share insights and advocate for the best possible terms. By working together, you can create a contract that benefits everyone and promotes a healthier healthcare industry overall.
We offer our provider credentialing service as an integrated part of our coding and billing service. Credentialing often leads to payer contracts that set rates and billing rules. We verify contract status, collate your payer contracts, and obtain fee schedules for each payer.
We are here to offer you a comprehensive suite of services to help you navigate the often complex and time-consuming provider credentialing and insurance application process.
Our services for Provider Credentialing include:
License and ID verification for clinical privileges, including telemedicine
Thorough verification of your licenses, certifications, Drug Enforcement Agency IDs, and National Provider Identifications (NPIs). This ensures that your credentials are up to date and compliant with all applicable regulations. Assistance for newly licensed clinicians in obtaining their NPIs, which is a critical step in the credentialing process.
Document collection for medical staff
Collection and secure storage of all supporting documents required for provider credentialing applications, such as driver’s licenses, birth certificates, Social Security numbers, diplomas, and curriculum vitae. This ensures that you have all the necessary documentation in one place and that it is kept safe and confidential.
Application submission
Preparation of separate application packets for every government and commercial insurance carrier, and submission of the applications on your behalf. This saves you time and effort and ensures your applications are completed accurately and submitted on time.
Payer follow-up for clinical privileges
Follow up with insurance carriers to confirm receipt of applications, respond to requests for additional information, and track application processing to ensure timely approval. This ensures that your applications are being processed and approved as quickly as possible.
Re-credentialing
Confirmation and maintenance of credential approvals, and re-credentialing on the provider’s behalf as needed. This ensures that your credentials remain current and that you can continue providing quality care to your patients.
What Provider Credentialing Covers Summary List
- Licenses
- Education
- Background checks
- NPI
- DEA, where applicable
- Medical Bylaws
- Peer Review
- Clinical Competency
- Disciplinary History
Who We Serve
Since 1977, we have served independent physicians and clinics across the Central United States. As a Silent Partner for Independent Physician Groups, the ebix team of expert medical billing service professionals helps keep your medical practice autonomous and realize up to 10% more revenue by focusing our efforts on coding expertise, denials minimization, and data analytics & reporting.
Frequently Asked Questions About Provider Credentialing
What is provider credentialing?
Provider credentialing is the process insurance companies use to verify a healthcare provider’s qualifications. This includes confirming licenses, education, background, and key identifiers to ensure the provider meets payer requirements and receives reimbursement for services.
Why do insurance companies require credentialing?
Payers require credentialing to confirm a provider is qualified and eligible to participate in their network. It also helps insurers set up the provider for claims payment under the payer’s rules, including CMS requirements, once the provider is approved.
What documents and information are commonly required for credentialing?
Credentialing often requires State Licensure, Board Certification, work history, malpractice history, background checks, and National Practitioner Data Bank queries. Supporting documents can include DEA information (when applicable), an NPI, a driver’s license, a birth certificate, a Social Security number, a diploma, a curriculum vitae, and other payer-specific forms.
What does ebix, Inc. do during the credentialing process?
The ebix, Inc. credentialing team verifies licenses, certifications, DEA IDs, and NPIs. The team collects and securely stores supporting documents, prepares payer-specific application packets, submits applications, and follows up with carriers to confirm receipt and address requests for more information.
Do providers need Recredentialing after initial approval?
Yes. Credentialing does not end at approval. Providers may need Recredentialing to keep payer approvals current. ebix, inc. helps maintain credential approvals and manages recredentialing on the provider’s behalf when needed, adhering to industry standards like those from The Joint Commission and NCQA.
Download Brochure ebix Physician Credentialing PDF
Get Started: Contact us for a Complimentary Consultation. Contact us today at sales@ebixinc.com / 877-991-6300