When a Hybrid Billing Model Beats Fully In-House Billing
Hybrid billing beats fully in-house when claim denials are up, billing staff turnover is constant, and cash flow feels slower than it should. If that sounds familiar, you’re not alone; many doctor offices, clinics, and medical practices are doing great patient care, but revenue cycle management (RCM) keeps getting heavier.
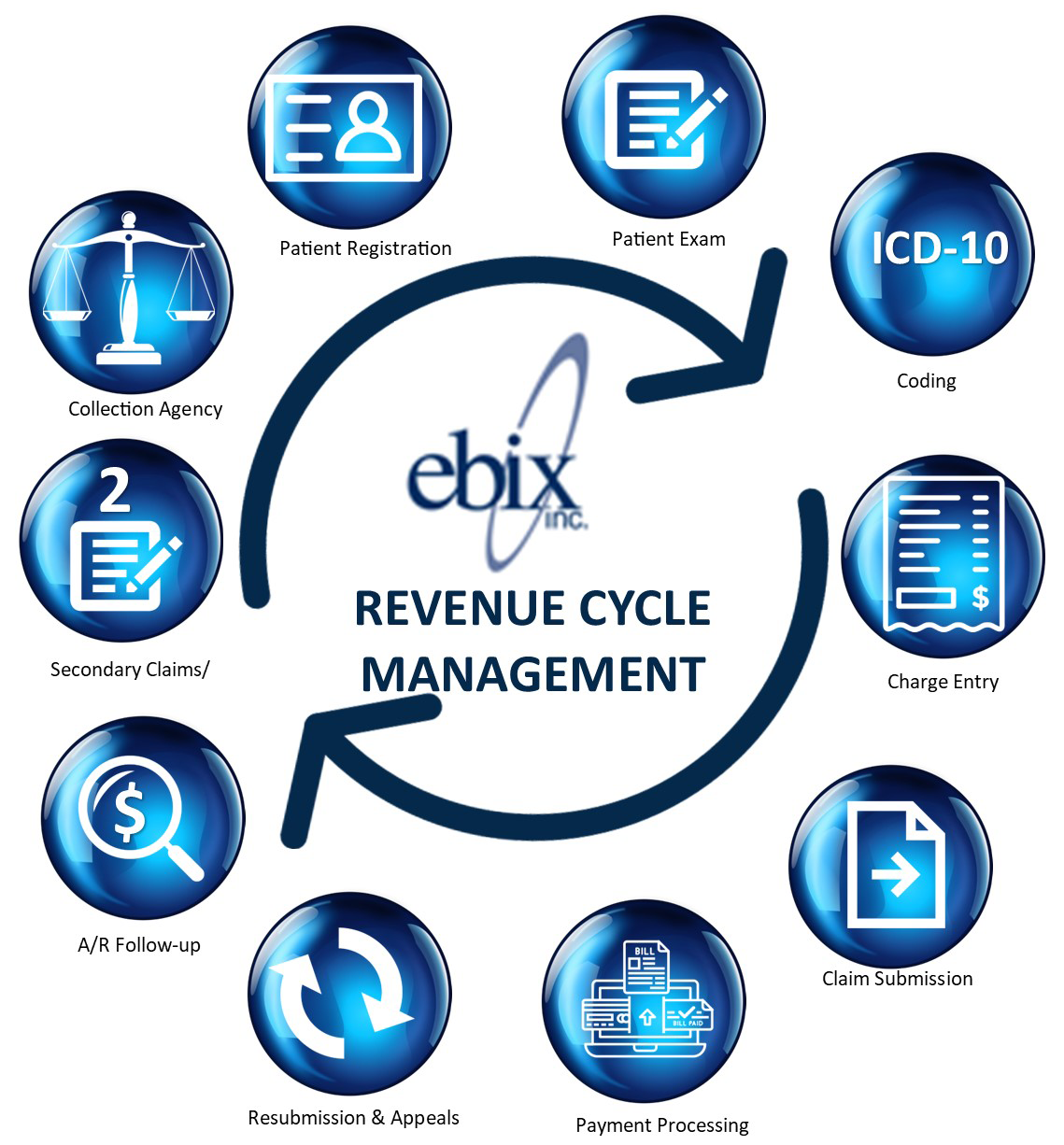
Fully in-house billing means your clinic’s own team handles billing and coding tasks from start to finish. A hybrid billing model splits the work, your clinic keeps key patient-facing steps, and an outside billing partner takes on the parts that usually bog teams down (coding support, claim work, denials, and A/R follow-up). Successful Hybrid RCM Model begins with ebix, Inc.
Many doctors offices and clinics choose ebix, Inc. because they want consistent follow-up, compliance-focused processes, coding and billing expertise from medical billing specialists, clear reporting, and support that can scale as the practice grows.
Key takeaways for doctors offices and clinics choosing hybrid medical billing
- Hybrid medical billing works best when your front desk is strong, but A/R is falling behind.
- The process helps when turnover, PTO, and training time keep creating billing gaps.
- This solution has its growth, new locations, and service expansion without constant hiring.
- The strategy adds coding support when accuracy issues cause denials or missed revenue.
- hybrid billing keeps control through shared KPIs, dashboards, and agreed handoffs.
This guide explains when hybrid beats fully in-house, what to keep in your clinic, what to hand off, and how to decide with real numbers, not guesswork.
Hybrid billing vs fully in-house billing, what is the real difference?
Think of billing like running a relay race. The baton is the claim. In-house billing means your team runs every leg. Hybrid means your team runs the first leg (patient access and clean intake), then you pass the baton to specialists who run the harder parts of billing and coding (coding, payer follow-up, denials, appeals).
Fully in-house billing, a simple workflow
In many clinics, the flow looks like this:
- Front desk checks in the patient, verifies insurance, collects copays.
- Staff gathers documentation, providers finalize notes.
- Coders or billers assign codes, enter charges, and create claims.
- Claims go out, then staff works rejections, denials, and appeals.
- Payments are posted, balances are worked, patient statements are handled.
- Reporting is created, often in spare moments or at month-end.
This represents the full revenue cycle handled entirely by internal teams. It can work well, but only if you have enough trained people, strong oversight, and time to keep up with payer rule changes.
Industry Data: According to a 2023 survey by the Healthcare Financial Management Association, practices using a hybrid billing RCM model reported an average 18% increase in net collections and a 25% reduction in denial rates compared to those managing RCM entirely in-house.
Actual Case Study: A 2024 report in RevCycle Intelligence detailed the experience of a 50-physician orthopedic group that implemented a hybrid billing RCM model. By outsourcing pre-authorization and claims follow-up while keeping coding and charge entry in-house, they achieved the following results over 18 months:
- 22% increase in net collections
- 35% reduction in denial rates
- 18-day decrease in average days in A/R
- $3.5 million improvement in annual revenue
The practice used the additional revenue to invest in a state-of-the-art MRI machine, which improved diagnostic capabilities and enhanced patient care through reduced patient wait times for imaging services.
Hybrid billing, a simple workflow
A common hybrid flow looks like this:
- Your clinic handles check-in, eligibility, copays, and documentation capture.
- Your team confirms charges are complete and ready to bill (or shares them with the partner for review).
- The billing partner supports coding, scrubs and submits claims, and works payer follow-up.
- Denials and appeals are managed by the partner with clear escalation rules.
- Reporting and KPI reviews happen on a set cadence (weekly or monthly).
This hybrid approach splits the revenue cycle, with your front end leading into partner expertise. Hybrid often works best when your clinic wants control over patient experience, but needs stronger follow-through on the back end.
What stays in your clinic with a hybrid model
In a strong hybrid setup, the clinic usually keeps responsibilities that affect patient trust and point-of-service collections:
Patient check-in and registration: This is where errors start, wrong policy numbers, outdated addresses, missing referrals.
Eligibility checks and authorizations: Done right, this prevents avoidable denials.
Collecting copays and estimating patient responsibility: It’s harder to collect after the visit than during it.
Documentation capture and provider queries: Your in-house staff is closest to the healthcare providers and the clinical story, so clarifying missing details is faster.
Charge entry review (or charge reconciliation): Many clinics keep the habit of confirming every visit becomes a billable charge, with in-house staff overseeing this step.
Keeping these steps internal reduces back-and-forth and protects the patient experience. It also helps your partner work faster because the “inputs” are cleaner.
What an outside billing partner typically handles
The partner’s role usually centers on work that needs depth, repetition, and payer persistence:
Coding support and audits: Specialty coding, E/M checks, CPT codes, and consistent review.
Claim scrubbing and submissions: Catching errors before they turn into denials.
Payer follow-up and A/R worklists: Calling, portal work, and tracking payer timelines.
Denials management and appeals: Root-cause analysis, resubmits, appeal letters, and follow-through.
Payment posting support and reconciliation: Matching payments, adjustments, and identifying underpayments.
A/R cleanup projects: Tackling old balances, filing limits issues, and stuck claims.
Compliance and rule updates: Keeping pace with payer edits, coding guidance, and documentation expectations.
Scope varies by vendor, so it needs to be spelled out in the service agreement, including turnaround times and who owns each task.
Actual Case Study: A 2023 case study published in MGMA Connection detailed a 100-provider primary care network’s experience with a hybrid RCM model. By implementing a shared workflow between in-house staff and an outsourced RCM partner, they achieved:
- 40% reduction in claim errors
- 25% improvement in first-pass resolution rates
- 30% decrease in patient wait times for billing-related queries
- 18% increase in overall patient satisfaction scores related to billing and financial processes
In another example, an orthopedic group implemented a hybrid RCM model, outsourcing eligibility verification and claims scrubbing while keeping coding and payment posting in-house. This resulted in a 30% reduction in claim errors and a 20% increase in first-pass resolution rates.
When does a hybrid billing model beat fully in-house billing?
Hybrid is not a “one-size” answer. It wins when you have specific pressure points and want measurable improvement, such as lower denial rates, higher clean claim rates, fewer A/R days, less staff overtime, and better financial performance.
You have strong patient service staff, but weak A/R and denials follow-up
Many clinics shine at the front desk. Phones get answered, schedules stay full, and patients feel cared for.
Then claims hit the payer wall. Follow-up slips are time-consuming and easy to postpone. A hybrid model adds dedicated A/R focus without forcing you to replace your entire billing team. You keep the people who are great with patients, and you add medical billing specialists who live in payer portals and denial codes all day.
Actual Case Study: According to a 2022 article in Healthcare Finance News, a 250-bed hospital in Florida implemented a hybrid billing RCM model to address staffing shortages. By outsourcing 70% of their billing and coding functions, they reduced staffing costs by $1.2 million annually while improving claim submission times by 35%. This allowed them to reallocate resources to patient care initiatives, resulting in a 15% increase in patient satisfaction scores.
Another example comes from a multi-specialty clinic in Texas that adopted a hybrid billing RCM model, outsourcing 60% of its billing functions while retaining a core in-house team. This approach reduced staffing costs by 30% and improved claim submission times by 40%.
Your clinic is growing, adding locations, or expanding services
Growth is exciting, but it also multiplies complexity. More providers often means more templates, more coding patterns, and more chances for charge lag. More locations can mean more registration variation, more payer plans, and more reporting needs. Expanding services like telehealth services adds even more billing complexity.
Hybrid can scale without constant hiring, boosting operational efficiency. You can expand visit volume while keeping billing capacity steady, as long as you set expectations on turnaround and reporting. This is especially helpful for multi-provider or multi-specialty practices where denial reasons differ by service line, such as remote patient monitoring.
You need better billing and coding accuracy or specialty coding support
Coding rules change often, and payer edits change even faster. Small errors create denials, but “quiet” errors can be worse, like undercoding that leaves revenue on the table.
Hybrid can bring certified coding expertise and routine audits while your clinic keeps control of clinical documentation workflows. That balance matters. Providers shouldn’t feel like outsiders are rewriting notes, but they should get clear feedback when documentation doesn’t support the billed service.
If you’re weighing how coding support can improve both compliance and revenue, this resource explains the benefits of medical coding services in practical terms.
You want control and transparency, but you need expert help
A common fear is losing visibility. With the wrong vendor, that can happen. With a good hybrid setup, you keep control through shared reporting, clear KPIs, and regular check-ins.
Look for basics that drive trust:
- Weekly huddles for stuck issues and top denial reasons
- Shared dashboards for A/R aging and payer trends
- Written definitions for “worked claim” and escalation rules
Hybrid should feel like a managed extension of your team, not a black box.
How to choose the right hybrid setup and avoid common mistakes
The biggest hybrid failures usually come from fuzzy handoffs, unclear scope, or poor reporting. The fix is simple: define the split, define the handoff, then measure it.
Pick your split, front-end vs back-end, then define the handoffs
Common splits include:
Clinic front-end, partner back-end: You handle registration and collections, partner handles claims and A/R.
Clinic keeps charge entry, partner handles A/R: Good when charges are solid, but follow-up is weak.
Partner supports coding only: Useful when denials trace back to coding issues.
Whatever you choose, document handoffs, who touches the claim next, how fast, and what happens when info is missing. Without that, claims fall into the cracks between teams.
Track the KPIs that show if hybrid billing is working
Baseline your numbers before you change anything. Then track simple metrics that connect to cash flow, with a focus on denial management:
- Clean claims rate
- First-pass acceptance rate
- Denial rate (and top denial reasons)
- Days in A/R
- Percent of accounts receivable over 90 days
- Net collections rate
- Charge lag (date of service to claim submission)
- Payment posting lag
- Appeal turnaround time
- Patient balance aging
If the hybrid is working, you should see fewer “mystery balances,” faster movement in accounts receivable, and less panic at month-end.
Actual Case Study: A 2024 article in Becker’s Hospital Review highlighted a 200-bed community hospital that partnered with an RCM analytics firm as part of its hybrid approach. Using advanced data analytics, they uncovered $3.2 million in missed charges over a 12-month period. Additionally, the insights gained led to a restructuring of their service lines, resulting in a 15% increase in high-margin procedures and a 10% improvement in overall patient throughput.
In another case, a cardiology practice working with an RCM partner gained insights into their payer mix and reimbursement trends. Using this data, they renegotiated contracts with key insurers, resulting in a 12% increase in average reimbursement rates.
Questions to ask any billing partner before you sign
Ask direct questions, and listen for direct answers:
Specialty fit: Have you billed for our specialty and payer mix?
Denials process: How do you categorize, work, and trend denials?
Coding credentials: Who codes our CPT and HCPCS codes, what credentials do they hold, and how are audits handled?
Compliance and HIPAA: What safeguards do you use against surprise medical billing, and how do you train staff?
Payer portal work: Who handles portals, and how do you document activity?
Reporting: What reports do we get, how often, and can we access raw data from our EHR systems?
No Surprises Act disputes: How do you handle out-of-network surprise medical billing disputes, including independent dispute resolution, arbitration, and benchmark payment?
Point of contact: Who owns day-to-day issues, and what’s the escalation path?
Implementation: What’s the timeline, and what do you need from our clinic weekly?
Pricing: What’s included, what’s extra, and how do you handle cleanup work
FAQs about hybrid billing for doctors and clinics
What is hybrid medical billing?
It’s a split model where your clinic keeps key front-end tasks, while a billing partner handles some or most back-end billing work. The goal is better collections without giving up patient experience control.
Is hybrid billing cheaper than fully in-house?
Sometimes, but “cheaper” isn’t the best test. Compare total cost, including turnover, training, overtime, missed collections from slow follow-up, and reimbursement rates.
Will we lose control of our billing?
Not if you set the split clearly and require reporting access. A good hybrid model improves visibility because work is tracked and reviewed on a schedule.
How fast will we see results?
Some clinics see early wins in 30 to 60 days, like fewer rejections and faster claim movement. Larger A/R cleanup and denial trend changes often take 60 to 90 days.
What data access do we keep?
You should keep access to your practice management system reports, claim status, and A/R aging. Also ask for documentation of payer outreach and denial notes.
How does HIPAA work with a billing partner?
The partner should sign a Business Associate Agreement and follow HIPAA security rules. You should also confirm training, access controls, and audit trails.
What should we keep in-house?
Most clinics keep patient-facing steps, eligibility, copays, and documentation requirements. Those items protect patient trust and keep claims clean from the start.
Call to action: decide if hybrid billing is right for your clinic
Pull your last 90 days of denials and your A/R aging report. Then pick one service line and trace what’s slowing payment, charge lag, missing info, coding edits, or follow-up gaps. If the pattern is clear, schedule a billing and coding review and ask what a hybrid scope would look like with measurable KPIs and steady follow-up for your medical practice. Finally, our medical billing consulting services provide a range of professional management services to medical providers throughout the Midwest. Potentially increase revenue by up to 10%. Contact us today at sales@ebixinc.com / 877-991-6300 for a complimentary consultation.
Conclusion
If your patient-facing work is strong, but collections and denials are slipping, hybrid medical billing can beat fully in-house billing. The right split boosts financial performance, improves cash flow, lowers staff stress, and keeps compliance solid. Review your revenue cycle management KPIs, and if gaps show up, talk with a partner and put the handoffs in writing.