Revenue Cycle Management: When You Need Quick Payments
Key Takeaways: Revenue Cycle Management for Independent Physicians
- Revenue Cycle Management (RCM) helps independent physicians get paid faster and maintain steady cash flow.
- Strong Revenue Cycle Management (RCM) reduces denied claims, fixes billing errors, and cuts time spent on paperwork.
- ebix Revenue Cycle Management (RCM) connects with EHR systems, automates key tasks, and supports accurate medical coding.
- Real-time reporting and simple tools help doctors spot problems early and make better decisions.
- Practices that use ebix Revenue Cycle Management (RCM) often see higher collections, fewer denials, and less staff stress.
Revenue Cycle Management (RCM) service powers independent doctors’ success. It puts cash in the bank faster and helps offices run better every day.
What is a revenue cycle management service for independent physicians?
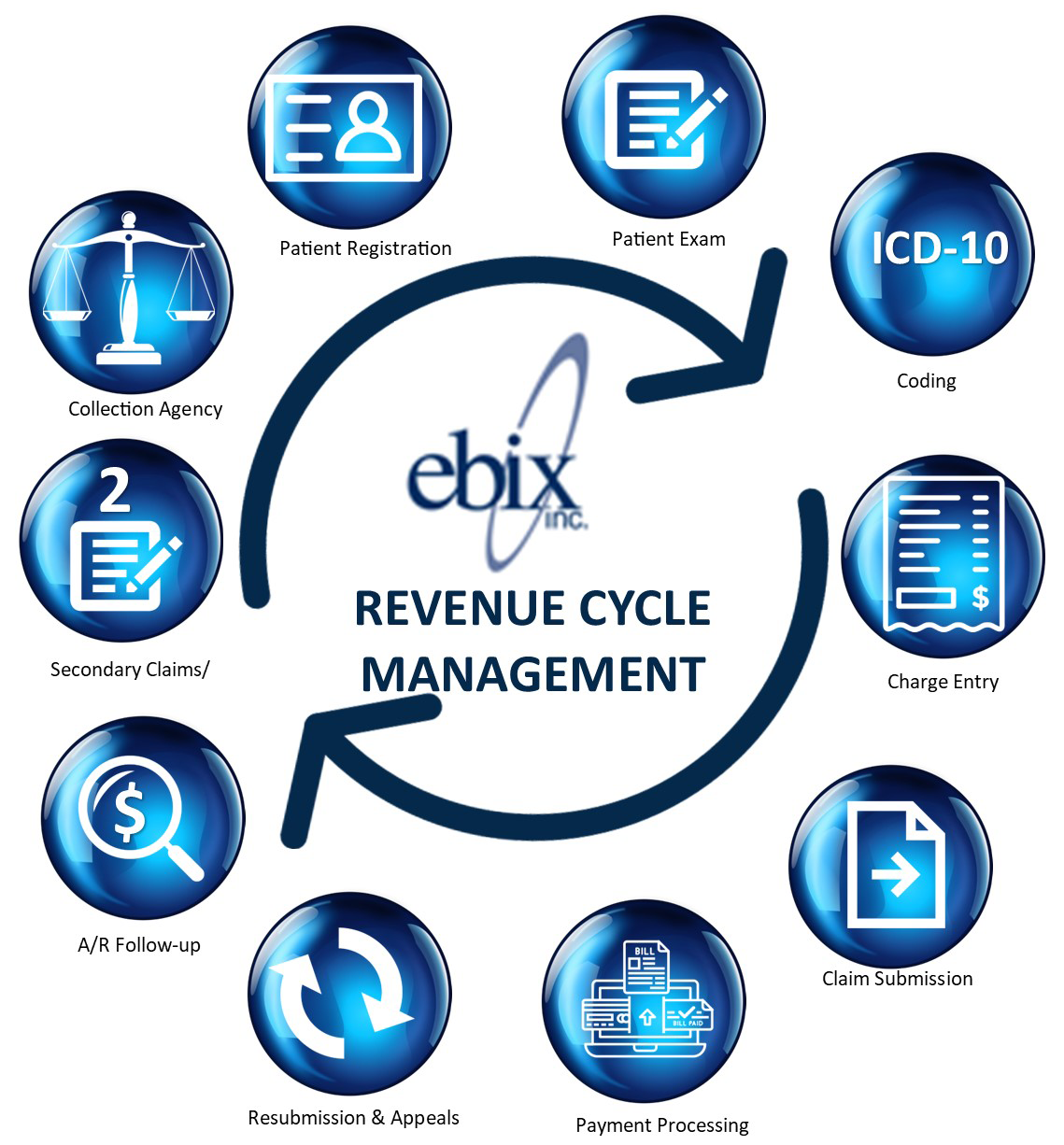
Revenue Cycle Management is the full process that moves a medical visit into a payment. It covers scheduling, insurance checks, coding, claim submission, payment posting, and follow-up on balances. When independent physicians understand these steps, they identify weak points, eliminate delays, and achieve more reliable income.
How does strong revenue cycle management help independent practices get paid faster?
Strong Revenue Cycle Management reduces errors before claims go to payers. Clean claims get paid sooner, and fewer are returned denied. Automation handles routine tasks such as scheduling, eligibility checks, and claim filing, so staff can respond more quickly when problems arise. This steady flow of clean claims leads to faster payments and more substantial cash flow.
What common revenue cycle problems do independent doctors face?
Independent doctors often feel buried in billing rules, codes, and forms. Staff spend significant time on booking, insurance questions, claim filing, and chasing balances. Small errors or missing details can cause denials and long payment delays. These problems hurt cash flow and pull attention away from patient care.
 How does ebix revenue cycle management help independent Physicians?
How does ebix revenue cycle management help independent Physicians?
Because ebix Revenue Cycle Management gives doctors more control and less stress, billing moves smoothly. Therefore, fewer claims get denied or delayed. Income builds up fast.
Automation lowers the workload. Tasks like scheduling, insurance checks, and claim filing take less time. The team can help patients instead of doing paperwork.
Patients notice the difference. More online options for visits and bills make life easier. Reminders cut no-shows and help bills get paid on time.
Real-time reports show doctors what’s working and what needs attention. Moreover, tracking details helps doctors spot issues and fix them early.
The ebix approach supports compliance. Doctors stay up to date on coding rules and privacy laws so audits don’t cause worry.
How does ebix revenue cycle management improve billing performance?
The ebix RCM Service connects with a practice’s EHR system, so staff avoid re-entering data. Claims scrubbing tools catch common coding and data errors before claims go out. Certified coders support accurate ICD-10 coding, which lifts payment rates and reduces denials. Real-time reports give doctors clear insight into cash flow, accounts receivable, and problem areas. The result is smoother billing and a more stable practice.
What results have practices seen using the ebix RCM service?
The article highlights independent physicians who achieved strong gains with ebix RCM service. Hence, one solo practice cut claim denials by 30 percent and increased revenue by 20 percent in one year. Another group practice cut accounts receivable time in half, easing stress and supporting growth. In general, doctors using ebix services see an average 10 percent increase in payments.
Revenue Cycle Management (RCM)Services
- Start credentialing for free. Our team calls insurers to help doctors join networks.
- We review fee schedules and contracts to spot underpayments or errors. We help set the appropriate service charge levels.
- Moreover, our management team builds intelligent workflows and trains your staff to do the right things every time.
- We scan insurance contracts and prevent problems before they start. More experts step in if any significant issues pop up.
- Certified coders review each claim to improve accuracy. We offer chart checks and staff training. This captures more revenue and protects your practice in audits.
- You only pay when we deliver results. No hidden fees for mail, statements, claims, or reports.
- We submit claims quickly so you don’t risk lost income.
- Doctors using our services see an average 10 percent increase in payments.
- Finally, ebix is a proud founding member of Independent Health Advisors and Independent Physician Advisors, and part of the Wisconsin Chapter of the American Association of Healthcare Administrative Management.
Who We Serve
Since 1977, we have served independent physicians and clinics across the Central United States. As a Silent Partner for Independent Physician Groups, the ebix team of expert medical billing service professionals helps keep your medical practice autonomous and realize up to 10% more revenue by focusing our efforts on coding expertise, denials minimization, and data analytics & reporting.