Provider Credentialing: What You Need to Know Now
The first thing to remember is that initial Provider Credentialing is Free. Our expert staff reaches out to the carriers of your choice to obtain network status. Free at startup and a very reasonable fee per provider afterward.
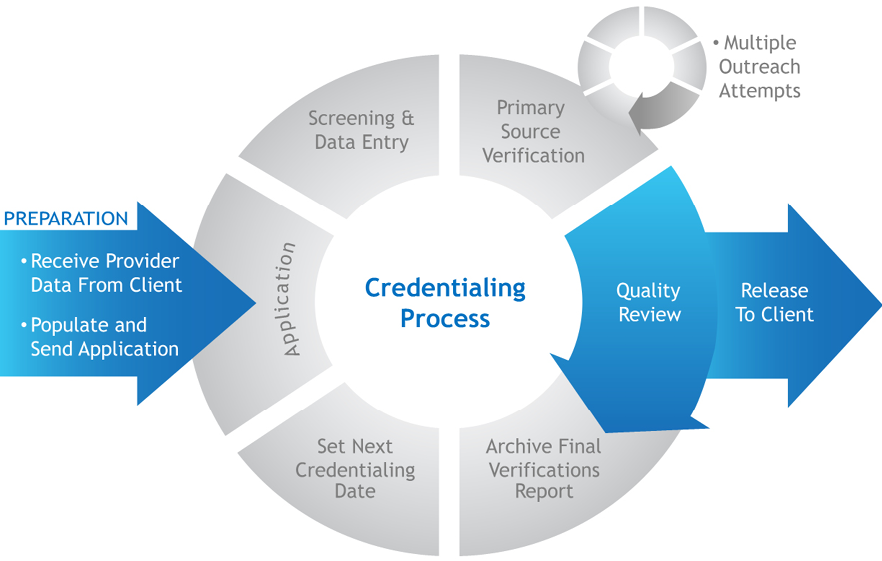
Generally speaking, Insurance companies use provider credentialing to assess the medical qualifications of healthcare providers and ensure they can receive payment for their services. It’s a thorough process to make sure the healthcare provider you see is qualified to give you the care you need. So, always ensure that your healthcare provider has undergone this process before seeking medical services from them. It’s the first step of, and the foundation for, all your interactions with governmental and private payers. It’s the process insurance companies employ to verify your physician’s licenses, education, background, and other information.
Furthermore, as you go through the credentialing process, you’ll be creating a contract that establishes the reimbursement rates and billing guidelines. This is an important opportunity to ensure that your compensation is fair and accurately reflects the value of your services. Consider collaborating with your colleagues to share insights and advocate for the best possible terms. By working together, you can create a contract that benefits everyone and helps to promote a healthier healthcare industry overall.
 Hence, we offer our credentialing service as an integrated part of our coding and billing service. We verify contract status, collate your payer contracts, and obtain fee schedules for each payer.
Hence, we offer our credentialing service as an integrated part of our coding and billing service. We verify contract status, collate your payer contracts, and obtain fee schedules for each payer.
We are here to offer you a comprehensive suite of services to help you navigate the often complex and time-consuming process of credentialing and insurance application.
Our services for Provider Credentialing include:
– Thorough verification of your licenses, certifications, Drug Enforcement Agency IDs, and National Provider Identifications (NPIs). This ensures that your credentials are up-to-date and compliant with all applicable regulations.
– Assistance for newly licensed clinicians in obtaining their NPIs, which is a critical step in the credentialing process.
– Collection and secure storage of all supporting documents required for credentialing applications, such as driver’s licenses, birth certificates, Social Security numbers, diplomas, and curriculum vitae. This ensures that you have all the necessary documentation in one place and that it is kept safe and confidential.
– Preparation of separate application packets for every government and commercial insurance carrier, and submission of the applications on your behalf. This saves you time and effort and ensures that your applications are completed accurately and submitted in a timely manner.
– Follow-up with insurance carriers to confirm receipt of applications, respond to additional information requests, and track application processing to ensure timely approval. This ensures that your applications are being processed and approved as quickly as possible.
– Confirmation and maintenance of credential approvals, as well as re-credentialing on the provider’s behalf as needed. This ensures that your credentials remain current and that you are able to continue providing quality care to your patients.
Contact us for a Complimentary Consultation.